Point-of-Care Hemostatic Testing for Transfusions and Blood Management
-
Patient Blood Management
PBM is a patient-centered, systematic, evidence-based approach to improve patient outcomes by managing and preserving the patient’s own blood.(4) Implementation of PBM programs have been shown to decrease blood product usage, decrease adverse outcomes and reduce costs.(5) The World Health Organization (WHO) issued a Policy Brief in 2021 on the urgent need to implement PBM in all member states.(6)
-
Optimizing coagulopathy
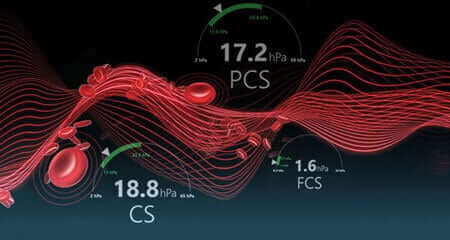
Is an important component of implementing a PBM program.(7) This requires rapid and accurate assessment of a patient’s coagulation status which favors whole blood point-of-care viscoelastic testing (VET)(8) :
- Compared to conventional laboratory-based coagulation testing, VET has the advantage of a rapid turnaround time with display of all phases of coagulation – from clot initiation to lysis (9).
- In guiding individualized hemostatic intervention in severely bleeding patients, VET is preferred over conventional coagulation testing because it has been shown to improve patient outcomes, reduce unnecessary blood product usage, and lower costs(10-15) .
- Compared to conventional laboratory-based coagulation testing, VET has the advantage of a rapid turnaround time with display of all phases of coagulation – from clot initiation to lysis.(9)
- In guiding individualized hemostatic intervention in severely bleeding patients, VET is preferred over conventional coagulation testing because it has been shown to improve patient outcomes, reduce unnecessary blood product usage, and lower costs.(10-15)
Recommendations from Medical
Societies for POC guided transfusions
Cardiothoracic surgery
Trauma
American College of Surgeons (ACS)
pan-European, multidisciplinary Task Force for
Advanced Bleeding Care in TraumaLiver transplantation
Anesthesiology
American Society of Anesthesiologists (ASA)
European Society of Anaesthesiology and
Intensive Care (ESAIC)European Association of Cardiothoracic
Anaesthesiology and Intensive Care (EACTAIC)
References: 1. Ferraris V, et al. Surgical outcomes and transfusion of minimal amounts of blood in the operating room. Arch Surg. 2012;147:49-55. 2. Saporito A, et al. Perioperative inappropriate red blood cell transfusions significantly increase total costs in elective surgical patients, representing an important economic burden for hospitals. Front Med. 2022;9:956128. 3. Ad N, et al. Number and type of blood products are negatively associated with outcomes after cardiac surgery. Ann Thorac Surg. 2022; 113:748-756. 4. Shander A, et al. A global definition of patient blood management. Anesth Analg. 2022;135:476-488. 5. Leahy MF, et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: a retrospective observational study in four major adult tertiary care hospitals. Transfusion. 2017;57:1347-1358. 6. World Health Organization (2021). The Urgent Need to Implement Patient Blood Management: Policy Brief. View 7. Meybohm P, et al. Patient blood management bundles to facilitate implementation. Tranfus Med Rev. 2017;31:62-71. 8. Society for the Advancement of Patient Blood Management (2019). Role of real-time/accurate diagnostic testing in patient blood management programs – point-of-care testing. View 9. Cohen T, et al. The strengths and weaknesses of viscoelastic testing compared to traditional coagulation testing. Transfusion. 2020;60(Suppl. 6):S21-S28. 10. Weber CF, et al. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012;117:531-547. 11. Pearse BL, et al. Protocol guided bleeding management improves cardiac surgery patient outcomes. Vox Sang. 2015;109:267-279. 12. Deppe AC, et al. Point-of-care thromboelastography/ thromboelastometry-based coagulation management in cardiac surgery: a meta-analysis of 8332 patients. J Surg Res.2016;203:424-433. 13. Redfern RE, et al. Thrombelastography-directed transfusion in cardiac surgery: Impact on postoperative outcomes. Ann Thorac Surg.2019;107:1313-1318. 14. Gonzalez E, et al. Goal directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg. 2016;263:1051-1059. 15. Leon-Justel A, et al. Point-of-care haemostasis monitoring during liver transplantation reduces transfusion requirements and improves patient outcome. Clin Chim Acta. 2015;446:277-283.
